IgG and IgA food antibody testing is one of the most controversial tools in digestive medicine.
Some providers dismiss it entirely ❌
Others misuse it—and unintentionally create fear around food 😟
Today, I want to explain why this testing can be extremely helpful—and why it absolutely requires expert interpretation.
I’ve been treating IBS for over 25 years and founded the IBS Treatment Center in 2005, where we’ve helped more than 10,000 patients recover. I’ve run IgG and IgA testing on every single one of them—so I’ve learned a few things about how this testing works in real patients, not just on paper.
You’ll often hear statements like:
“IgG just means you’ve eaten the food.” ❌
“IgA only reflects mucosal immunity.” ❌
These explanations are incorrect and misleading.
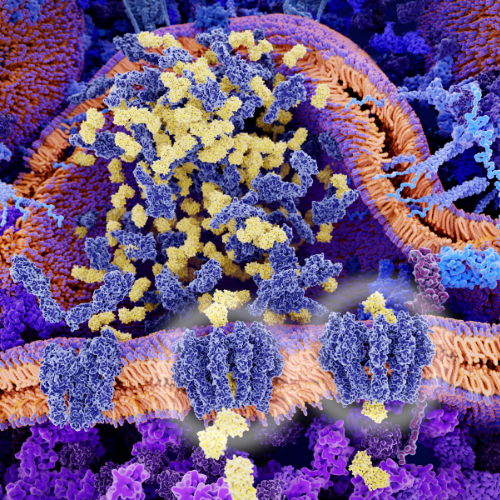
IgG and IgA antibodies are active components of the adaptive immune system. They participate in immune signaling, inflammatory responses, and immune–antigen interactions 🧬🔥
And importantly, IgG and IgA antibody testing is already used in conventional medicine, including in celiac disease—where both IgA- and IgG-based antibodies play a central role in diagnosis and monitoring 🩺
So the issue isn’t whether these antibodies are biologically meaningful.
👉 The issue is how the information is interpreted.
Many of the patients we see have already:
Yet they’re still symptomatic.
IgG and IgA testing helps identify immune-mediated food reactions that don’t show up as classic IgE allergies ⚠️
There are controlled studies showing that IgG-guided elimination diets can improve IBS symptoms compared to sham diets. More importantly, we’ve seen this clinically—thousands of times.
I’ve had patients eating very “clean” diets, doing everything right—yet still reacting.
When we used high-quality, reproducible antibody testing and interpreted it correctly, patterns emerged that finally explained why certain foods consistently triggered symptoms 🎯
Yes—IgA plays a major role at mucosal surfaces.
But clinically, it tells us much more.
IgA patterns can reflect:
In patients with long-standing IBS, autoimmunity, or chronic gut inflammation, IgA results can provide critical context—especially when interpreted alongside symptoms and clinical history 🧠
This is one of the most important points in this entire discussion.
If someone has significant gut inflammation or increased intestinal permeability, their immune system may be exposed to far more food antigens than normal.
When that happens:
I’ve seen patients arrive with pages of “positive” foods—convinced they’re intolerant to all of them.
In reality, another underlying issue was driving the inflammation.
Once that issue was addressed, many foods stopped causing problems—and antibody levels dropped. In other cases, only specific foods remained relevant triggers.
The test wasn’t wrong.
The interpretation just wasn’t complete.
This part matters.
Sometimes foods can be reintroduced ✅
And sometimes they can’t ❌
It depends on:
I’ve worked with patients who successfully reintroduced foods they hadn’t tolerated in years.
And I’ve worked with others where long-term avoidance was the right choice for staying symptom-free.
There is no universal rule—and blanket statements don’t work.
IgG and IgA food antibody testing is not a DIY tool.
Without proper interpretation, it can:
At the IBS Treatment Center, we use this testing as one piece of a much larger clinical picture.
We focus on:
That level of nuance only comes from experience—decades of it.
If you’re struggling with ongoing gut symptoms, there is more than hope.
For over 20 years, we’ve worked with patients around the world via telemedicine, helping them uncover the real drivers of their symptoms and move forward with clarity and confidence 🌍
And remember—take good care of your body.
It’s the only place you have to live. 💙
1) IgG-guided elimination diet improves IBS symptoms (classic RCT)
Atkinson W et al., 2004 (PMC) — Found that food elimination based on IgG antibodies may be effective in reducing IBS symptoms and worthy of further research. PMC
🔗 https://pmc.ncbi.nlm.nih.gov/articles/PMC1774223/
________________________________________
2) IgG levels are associated with intestinal permeability biomarkers
Vita AA et al., 2022 (PubMed / PMC) — Strong associations between food-specific IgG antibodies and biomarkers of intestinal permeability, suggesting relevance in conditions involving barrier dysfunction. PubMed+1
🔗 https://pubmed.ncbi.nlm.nih.gov/36147305/
🔗 https://pmc.ncbi.nlm.nih.gov/articles/PMC9485556/
________________________________________
3) Higher prevalence of food-specific IgG in IBS patients vs controls
Peruhova M et al., 2022 (PMC) — Found significantly higher and more frequent food-specific IgG in IBS patients than healthy controls, potentially linking immune responses to symptoms. PMC
🔗 https://pmc.ncbi.nlm.nih.gov/articles/PMC9036216/
________________________________________
4) Food-specific IgG antibodies in IBD patients suggest clinical utility
Cai C et al., 2014 (PLoS ONE) — Demonstrated a high prevalence of IgG antibodies to specific food antigens in patients with IBD, suggesting potential use in guiding diets. PLOS
🔗 https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0112154
________________________________________
5) IgG antibodies reported in multiple immune-related GI conditions
Tecan / IgG4 overview — Reports that specific serum IgG4 antibodies have been observed in celiac disease, IBS, and IBD, showing that IgG food antibodies are part of immune responses in GI disorders. Tecan
🔗 https://www.tecan.com/blog/igg-food-intolerance-blood-test-elisa
________________________________________
6) Associations between food-specific IgG and intestinal barriers/inflammation (review)
Garmendia JV et al., 2025 (MDPI Review) — Several studies link elevated food-specific IgG with conditions characterized by increased gut permeability and inflammation, including IBS and IBD, and discuss IgG-guided dietary interventions. MDPI
🔗 https://www.mdpi.com/2673-5601/5/3/25
________________________________________
7) Non-IgE mediated food immune disorders include antibody responses
Nowak-Węgrzyn et al., 2015 (JACI) — Describes non-IgE gastrointestinal food-induced allergic disorders (though not focused solely on IgG/IgA, it shows that immune responses beyond IgE matter clinically). JAC Online
🔗 https://www.jacionline.org/article/S0091-6749%2815%2900430-3/fulltext
________________________________________
8) Visualization of food reactions via confocal laser endomicroscopy in IBS
Fritscher-Ravens A et al., 2019 (Gastroenterology) — Using advanced imaging, this study showed many IBS patients have immediate mucosal responses to specific food components. This supports the concept of immune-related food reactions. Gastro Journal
🔗 https://www.gastrojournal.org/article/s0016-5085%2819%2934636-0/fulltext
________________________________________
9) Anti-gliadin IgA and IgG are central to celiac disease diagnosis
Anti-gliadin antibodies (Wikipedia summary) — IgA and IgG responses to gliadin are well-established markers in celiac disease, showing that both antibody types are clinically meaningful in immune-mediated food conditions. Wikipedia
🔗 https://en.wikipedia.org/wiki/Anti-gliadin_antibodies
________________________________________
10) Clinical overview of food allergy & intolerance evaluation
Onyimba F et al., 2021 (ScienceDirect) — A clinical article on evaluating adverse food reactions including immune-mediated pathways, useful for context on why broader antibody assessment (beyond IgE) can be relevant. sciencedirect.com
🔗 https://www.sciencedirect.com/science/article/pii/S1542356521000756
How Drug Companies Influence IBS Care (And All Care)
You’ve Been Diagnosed with IBS, Now What?
Seattle: 206-264-1111
Los Angeles: 310-319-1500
Our WhatsApp: 206-791-2660
Copyright © 2024 IBS TREATMENT CENTER. All Rights Reserved
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Suspendisse varius enim in eros elementum tristique. Duis cursus, mi quis viverra ornare, eros dolor interdum nulla, ut commodo diam libero vitae erat. Aenean faucibus nibh et justo cursus id rutrum lorem imperdiet. Nunc ut sem vitae risus tristique posuere.